
Chronic prostatitis is a serious problem. Even modern urology cannot answer many questions regarding this pathology. Experts believe that chronic prostatitis is a disease that is the result of a number of health problems, including tissue damage, as well as disorders not only of the urinary tract and prostate, but also of other organs.
The pathology is diagnosed mainly in men of reproductive age. In older men, chronic prostatitis is often accompanied by benign prostate neoplasms.
Classification of diseases
The classification of prostatitis was developed by scientists from the American National Institutes of Health in 1995:
%20and%20inflamed%20chronic%20prostatitis%20(right).webp)
- 1 type- acute bacterial prostatitis. It is diagnosed in 5% of cases of prostate inflammation.
- type 2- bacterial chronic prostatitis.
- 3 types- chronic bacterial prostatitis. This pathology has another name - chronic pelvic pain syndrome.
- 3A type- inflammatory form of chronic prostatitis. It is diagnosed in 60% of cases of chronic prostatitis.
- 3B type- non-inflammatory form of chronic prostatitis. It is diagnosed in 30% of cases.
- 4 types- asymptomatic prostatitis.
There is also a classification of chronic prostatitis, compiled in 1990.
Symptoms of chronic prostatitis
Feelings of discomfort and pain in the pelvic area that last longer than 3 months are the main symptoms of chronic prostatitis.
In addition, urinary disorders and erectile dysfunction are noted:
- pain occurs in the perineum, can radiate to the anus, groin, inner thighs, sacrum, lower back and scrotum. Pain on one side, extending into the testis, is often not a symptom of chronic prostatitis;
- erection does not occur, despite the presence of adequate conditions, but complete impotence is not observed;
- premature ejaculation is observed in the early stages of the disease;
- frequent urination, urinary incontinence, pain and burning in the process of emptying the bladder.
The clinical picture may vary depending on the type of chronic prostatitis.
infectious form:
- frequent urination at night;
- pain in the thighs, perineum, glans penis, and rectum, intensified by movement;
- painful urination;
- weak stream of urine.
Specific infectious:
- mucous discharge from the urethra;
- the above symptoms.
Non-infectious prostatitis:
- acute pain in the perineum;
- pain in the thighs and head of the penis;
- the pain is exacerbated by forced interruption of sexual intercourse or prolonged absence of intimate life.
Bitan!The disease progresses in waves. Symptoms can either weaken or intensify, but their presence clearly indicates the presence of an inflammatory process.
Symptoms may vary depending on the stage of pathology development.

The following stages of pathology development are distinguished:
- Exudative. The patient feels pain in the pubis, groin and scrotum. Frequent urination and a feeling of discomfort after intercourse occur. An erection can hurt.
- An alternative.The pain intensifies, is localized in the groin, pubic area and returns to the sacrum. Urination is accelerated, but it takes place without difficulty. Erection does not suffer.
- Proliferative.During exacerbation, urination becomes more frequent. The urine stream becomes weak.
- Cicatricial.Prostate tissue sclerosis occurs. There is a feeling of heaviness in the sacrum and pubic area. Increased urination. Erection becomes weak. Ejaculation may be completely absent.
Symptoms can vary depending on the course of the disease, but in each case it will gradually increase.
Causes of chronic prostatitis
There are many factors that lead to chronic prostatitis. The disease occurs under the influence of infectious agents. The patient has hormonal, neurovegetative, immune and hemodynamic disorders. Biochemical factors, urinary reflux into the prostate lobes, and dysfunction of growth factors, which are responsible for the proliferation of living cells, are affected.
Reasons influencing the occurrence of pathology:
- infections of the genitourinary system;
- hypodynamics;
- irregular sex life;
- continuous bladder catheterization;
- regular hypothermia.
Developmentdiseases of a bacterial naturestimulates intraprostatic urinary reflux.
Chronic abacterial prostatitisit develops against the background of neurogenic disorders of the pelvic floor muscles, as well as the elements responsible for the functioning of the bladder wall, prostate and urethra.
Formationmyofascial trigger points, which are located near the organs of the genitourinary system and prostate, can cause pelvic pain syndrome. Spots that result from certain diseases, surgeries, and injuries can cause pain in the pubic region, perineum, and adjacent areas.
Diagnosis of pathology
The presence of a complex of symptoms allows the diagnosis of chronic prostatitis without major difficulties. However, in some cases, the pathology may be asymptomatic. In this case, in addition to the standard examination and examination of the patient, additional research methods are needed.Neurological examination and examination of the patient's immune status is mandatory..
Bitan!Special questionnaires and questionnaires allow you to more accurately determine the subjective feelings of the patient and get a complete picture of the health condition, pain intensity, ejaculation disorders, erection and urination.
Laboratory diagnostics
Laboratory diagnostics enables the distinction between bacterial and abacterial forms of pathology, as well as determining the type of pathogen and making the most accurate diagnosis.Chronic inflammation of the prostate is confirmed when a fourth sample of urine or prostate secretion contains more than 10 leukocytes in PZ, or bacterial associations.When the leukocyte count is increased and bacteria are not inoculated, the material is examined to detect chlamydia or other sexually transmitted pathogens.
- The discharge from the urethra is sent to the laboratory to detect viral, fungal and bacterial flora, leukocytes and mucus in it.
- Scraping from the urethra is examined by PCR. This allows you to identify sexually transmitted pathogens.
- Perform a microscopic examination of prostate secretions to count the number of macrophages, leukocytes, amyloid and Trousseau-Lallemand bodies. An immunological study and a bacteriological study were prescribed. Determine the level of nonspecific antibodies.
- Blood sampling is performed ten days after digital rectal examination to determine the concentration of PSA in it. At a rate above 4. 0 ng / ml, the patient undergoes a prostate biopsy to rule out oncology.
The diagnosis is made based on the results of the research.
Instrumental diagnostics
Transrectal ultrasound of the gland will help to clarify the stage and form of the disease. Ultrasound allows you to rule out other diagnoses, monitor the effectiveness of treatment, as well as determine the size of the prostate, its echostructure, homogeneity and density of seminal vesicles. Urodynamic studies and myography of the pelvic floor muscles will allow the detection of infravesical obstruction and neurogenic disorders that often accompany pathology.
Tomography and MRI are used to make a differential diagnosis, especially in prostate cancer. These methods will reveal injuries to the pelvic organs and the spine.
Differential diagnosis
Differential diagnosis is important because there is a risk that the patient has a more serious illness.
The differential diagnosis is made with the following diseases:
- pseudodysynergia, functional disorder of the detrusor-sphincter system, urinary bladder dysfunction of neurogenic origin, complex regional pain syndrome;
- bladder stricture, hypertrophic changes in the bladder neck, prostate adenoma;
- pubic joint osteitis, cystitis;
- rectal pathology.
If symptoms occur, the prostate should be examined by a urologist or andrologist. Do an ultrasound examination. If necessary, a prostate biopsy is prescribed.
Methods of treating pathology
Chronic prostatitis is treated by a urologist or andrologist. Therapy is carried out in a complex way. Correction is subject to the patient's lifestyle, thinking characteristics and habits. It is important to move more, minimize alcohol intake, get rid of nicotine addiction, eat properly and normalize your sex life. However, without a course of basic therapy it will not work. Taking medication is the main condition for complete recovery.
Indications for hospitalization
Most often, treatment is performed on an outpatient basis. But in cases when the disease cannot be corrected and has a tendency to recur, the patient is referred to a hospital where treatment is more effective.
Medical method of treatment
This method is aimed at eliminating the existing infection, normalizing blood circulation, improving the drainage of the prostate lobules, correcting the hormonal background and immune status. Therefore, doctors prescribe antibiotics, vasodilators, immunomodulators, anticholinergics, and anti-inflammatory drugs.
If the pathology is bacterial in nature, antibiotics are definitely recommended. The drug is prescribed based on the results of the bacterial culture of prostate secretions.This will allow the isolation of the pathogen with the subsequent determination of its susceptibility to a particular drug. With a well-designed scheme, the effectiveness of treatment reaches more than 90%.
In the abacterial form, a short course of antibiotics is prescribed. It is continued only if the scheme gives a positive result. The effectiveness of the therapy is about 40%
In chronic pelvic pain, the duration of the course of antibiotics is not more than a month. With positive dynamics, treatment is continued for another month. If there is no effect, the drug is replaced by another, which may be more effective.
Antibacterial agents from the fluoroquinolone group are the main drugs for the treatment of pathology.They have high bioavailability, are active against most gram-negative bacteria, ureaplasma and chlamydia, and accumulate in prostate tissues.
When fluoroquinolone treatment is not effective, penicillins may be prescribed.
Antibacterial drugs are used for preventive purposes.
After treatment with antibiotics, α-blocker therapy is prescribed.This treatment strategy is effective for patients who have persistent obstructive and irritant symptoms.
If urination disorders and pain persist, tricyclic antidepressants that have an analgesic effect may be prescribed.
With severe urinary disorders, before starting therapy, a urodynamic study is conducted and acts on the basis of the results obtained.
Drug-free therapy
Drug-free therapy methods allow to increase the concentration of antibacterial drugs in the glandular tissues, but overdose is not recommended.
The following methods are used for this purpose:
- electrophoresis;
- Laser therapy;
- Phonophoresis;
- Microwave hyperthermia (applied transrectally).
When applying the last method, the temperature is selected individually. The temperature, set in the range of 39-40 degrees, allows you to increase the concentration of the drug in the body, activates the immune system at the cellular level, eliminates bacteria, and alleviates congestion. Increasing the range to 40-45 degrees allows to achieve a sclerosing and analgesic effect.
Laser and magnetic therapy are used in combination. The effect is similar to the effect of these methods, but it also has a biostimulating effect on the organ.
Transrectal massage is performed only in the absence of contraindications.
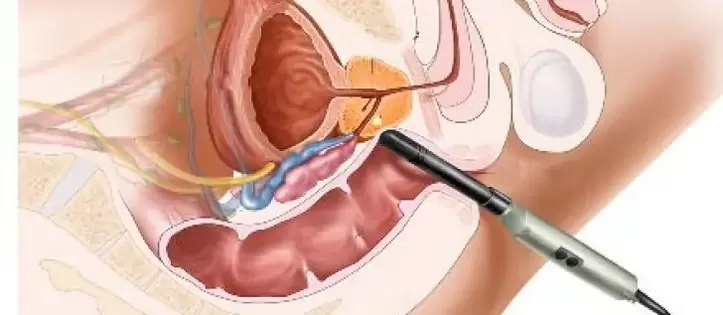
Surgical method
Chronic prostatitis generally does not require surgery. Exceptions are complications that pose a threat to the health and life of the patient. Modern surgical treatment enables the use of endoscopic surgery. It is minimally invasive. Rehabilitation is faster, and minimal damage is inflicted on the body.
The surgical method is prescribed for:
- prostate sclerosis;
- prostate adenoma;
- seminal tubercle sclerosis;
- calcification in the prostate.
Bitan!Surgery is contraindicated in the acute phase. Surgical treatment is prescribed by a surgeon based on the results of the study and the overall clinical picture.
Prognosis for chronic prostatitis
Doctors are careful in predicting the outcome of the disease. Rarely is a complete recovery achieved. Basically, chronic prostatitis goes into a phase of prolonged remission. The symptoms disappear, urine and blood counts return to normal. In order for chronic prostatitis not to become more active and not to cause complications, it is necessary to follow all the recommendations of experts.

























